Over several decades since 1981 we have learned to distinguish between one virus and the disease it can cause:
HIV: Human Immunodeficiency Virus, and
AIDS: Acquired ImmunoDeficiency Syndrome.
And of course over time scientists have identfied two main virus strains:
HIV-1 is more virulent, easily transmitted and is the cause of the vast majority of HIV infections globally.
HIV-2 is less transmittable and is largely confined to West Africa.
In the rush to inform people during this current pandemic, the terminology for public consumption has glossed over important distinctions between coronavirus, the Wuhan novel virus and the disease fatal to some people.
Some technical terminology from WHO: Naming the coronavirus disease (COVID-19) and the virus that causes it.
Coronaviruses
First characterized in the 1960s, these are a group of related viruses that cause diseases in mammals and birds. In humans, coronaviruses cause respiratory tract infections that can be mild, such as some cases of the common cold (among other possible causes, predominantly rhinoviruses), and others that can be lethal, such as SARS and MERS.
Novel coronavirus originating in Wuhan, China.
SARS-CoV-2 (Severe Acute Respiratory Syndrome CoronaVirus 2)
WHO’s International Committee on Taxonomy of Viruses (ICTV)announced “severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)” as the name of the new virus on 11 February 2020. This name was chosen because the virus is genetically related to the coronavirus responsible for the SARS outbreak of 2003. While related, the two viruses are different.
2019 Coronavirus Disease Pandemic
COVID-19 (COronaVIrus Disease 2019)
WHO announced “COVID-19” as the name of this new disease on 11 February 2020, following guidelines previously developed with the World Organisation for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO)
A Timeline of Historical Pandemics
(link goes to visualization by Flourish team)
Technical accuracy with these terms is important to understand testing and reports of the pandemic progress. A helpful guide is published in Scientific American today Here’s How Coronavirus Tests Work—and Who Offers Them. Excerpts in italics with my bolds.
PCR-based tests are being rolled out in hospitals nationwide, and the Food and Drug Administration is fast-tracking novel approaches as well
Virus Testing
The first step in any coronavirus test is collecting a sample. Doing so involves placing a sterile swab at the back of a patient’s nasal passage, where it connects to the throat via the nasopharynx, for several seconds to absorb secretions. Scott Wesley Long, a clinical microbiologist who directs Houston Methodist Hospital’s diagnostic microbiology lab, says the swab is thin—less than three millimeters in diameter at its tip. “Once you place it in the back of the throat, it’s uncomfortable, but you can still breathe and talk,” he says. “It’s not as bad as it looks.” After a sample is collected, the swab goes into a liquid-filled tube for transport.
To determine whether a nasopharyngeal sample is positive for the coronavirus, biotechnicians use a technique known as reverse transcriptase polymerase chain reaction, or RT-PCR. The World Health Organization’s and CDC’s test kits both use this method, as do all of the kits the latter has approved to date. [This detects signs of the virus’s genetic material.]
Stephanie Caccomo, a spokesperson for the FDA, says the positive predictive value, or likelihood a positive test result correctly reflects that a patient has COVID-19, depends on how widespread the disease is—and that situation is changing quickly. “Based on what is known about the pathophysiology of COVID-19, the data provided and our previous experience with respiratory pathogen tests, the false-positive rate for authorized tests is likely to be very low, and the true-positive rate is likely to be high,” Caccomo says.

Person loads a Mesa Biotech cartridge into a dock for testing. Credit: Mesa Biotech
On Saturday Cepheid, a Silicon Valley–based molecular diagnostics company, said the FDA had granted it authorization for a COVID-19 test that can deliver results in about 45 minutes. And on Tuesday Mesa Biotech in San Diego announced it had received the go-ahead for a handheld test kit that Hong Cai, the company’s CEO, says can deliver results at bedside in about half an hour. Cai says the tests will begin shipping this week to “several hospitals” and that her company has tens of thousands of units ready to go, adding that Mesa is planning to triple its production capacity.
Antibody Testing
Another approach relies on identifying antibodies to the coronavirus (SARS-CoV-2) in a patient’s bloodstream to determine whether that person previously had COVID-19. Florian Krammer, a microbiologist at the Icahn School of Medicine at Mount Sinai, recently developed one of these tests, which is described in a preprint study posted last week on medRxiv. “This is not a test for [ongoing] infections,” he says. “It basically looks for antibodies after the fact, after you had an infection.” Like other serological, or antibody-based, diagnostic assays, it uses an enzyme-linked immunosorbent assay (ELISA), which employs a portion of the target virus to find antibodies. Although serological tests are not useful for quickly identifying whether a patient currently has COVID-19, Krammer says they can help researchers understand how humans produce antibodies to the virus.
Additionally, serological tests can also help determine if a person has been infected whether or not the individual had symptoms—something an RNA test kit cannot do after the fact, because it only looks for the virus itself. That means serological tests could be used to survey a population to determine how widespread infection rates were. It also could allow public health agencies to figure out who is already immune to COVID-19. “So if you would roll this out on a very wide scale, you could potentially identify everybody who is immune and then ask them to go back to their regular life and go back to work,” Krammer says. This approach could be especially useful for health care providers who are working with COVID-19 patients. “They might feel much more comfortable working with those patients, [knowing] that they can’t get sick anymore, knowing that they can’t pass on the virus to others,” he says.
Comment:
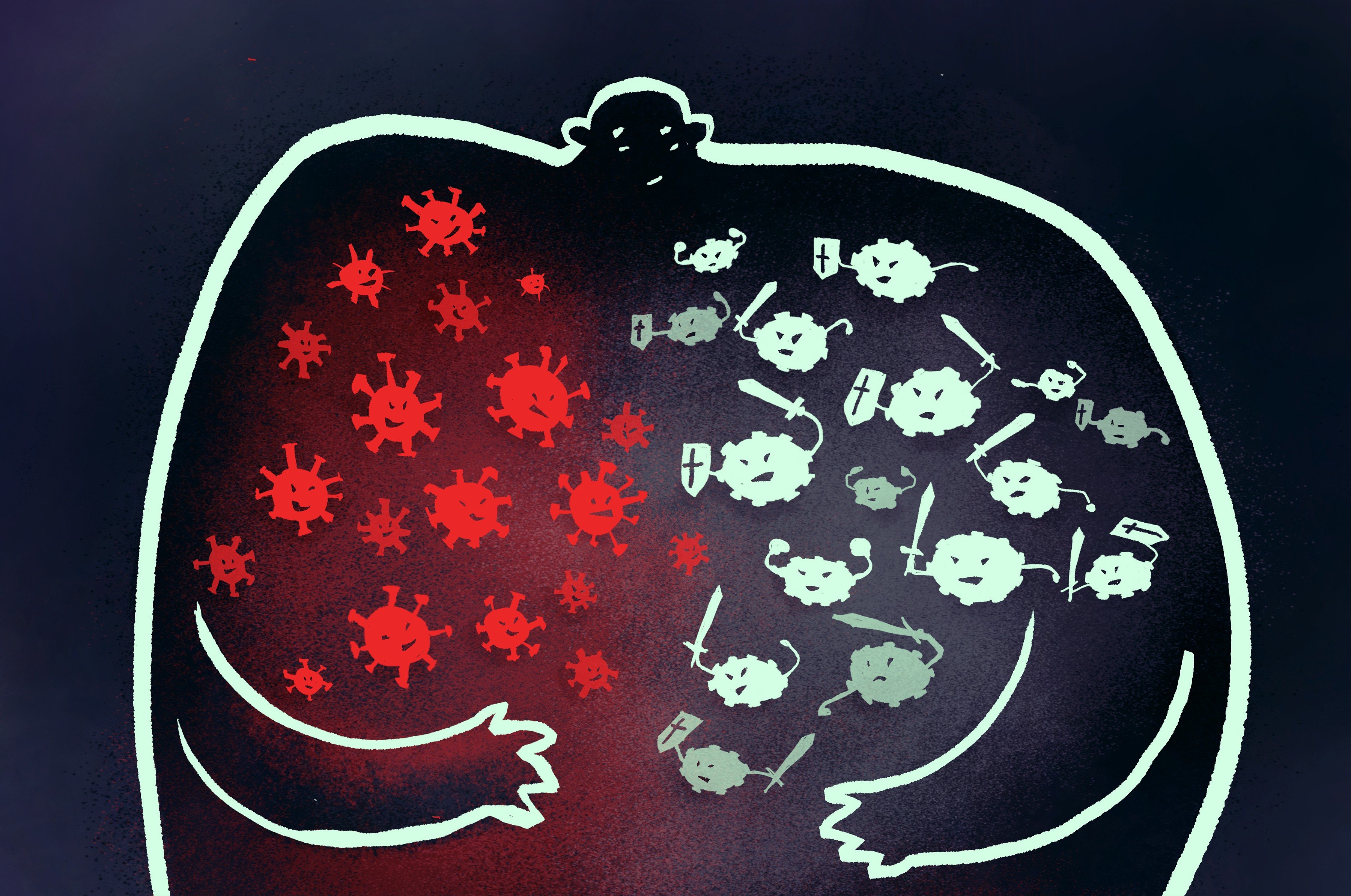
In common discourse, we talk about “disease” or “illness”, refering to how we feel, that is our awareness of symptoms. In fact, the entry of a virus (or other pathogen such as bacteria, fungi or parasite) sets up a battle with our immune system even before we know it. When the virus is defeated quickly, we have mild or no symptoms, and at least in the case of seasonal flus, we can be immune to further infection. In some cases, people weakened by fighting other pathogens will need hospital help and may not survive. The subtle point is that presence of the virus and the state of the disease are two different things.
This video is helpful in getting the basics right (published March 9, 2020)
See also: Progress on Covid19 Antibodies
Thanks for clarifications and update Ron!
CA’s testing is moving along-
https://calmatters.org/health/2020/03/california-coronavirus-test-results-delayed-backlog/
LikeLike
Thanks kakatoa. I see that Iceland may be showing the way to deal with this:
https://www.nbcnews.com/news/world/iceland-employs-detective-work-testing-quarantine-coronavirus-fight-n1170166
LikeLiked by 1 person
“But what makes Iceland unique is that test samples are not only taken from ‘high risk’ individuals who have exhibited symptoms, came into contact with known carriers, or returned from countries such as China and Italy, they are also offered to thousands of ordinary members of its general population, who are nonsymptomatic.
The data derived from this widespread testing show that while almost a fifth of those from the ‘high risk’ population prove positive for COVID-19, roughly 1 percent of the general population also carry the virus ‘asymptomatically’ — without showing or experiencing obvious signs of sickness.
Identifying these invisible and unwitting carriers early has helped to break chains of transmission in Iceland. But it could also provide scientists in many other countries with crucial information about the pathology of the virus.”
LikeLiked by 1 person
Reblogged this on HiFast News Feed.
LikeLike